CPAP vs BiPAP: Difference, Benefits, & Medicare Coverage Guide
Key Takeaways
- Pressure Functionality: The main difference is that CPAP provides a single, constant flow of air, whereas BiPAP uses dual pressure levels—higher for inhalation (IPAP) and lower for exhalation (EPAP).
- Ideal Candidates: CPAP is the standard first-line treatment for most Sleep Apnea patients, while BiPAP is specifically beneficial for those with high pressure needs, COPD, or difficulty breathing against constant pressure.
- Medicare Step Therapy: Medicare covers both machines but typically requires patients to attempt and fail a trial with a CPAP machine before they will approve the more expensive BiPAP option.
- Coverage Requirements: To qualify for 80% coverage under Medicare Part B, you must have a face-to-face doctor evaluation, a confirmed diagnosis from a sleep study, and a “Standard Written Order” (prescription).
- Compliance Rule: During the initial 12-week trial, you must use your machine for at least 4 hours per night for at least 70% of nights to maintain your insurance coverage.

Choosing the right equipment for sleep apnea therapy is a critical step in improving your health and sleep quality. While both machines provide life-changing benefits, understanding the difference between cpap and bipap is essential for ensuring your treatment is as comfortable as it is effective.
How Does a CPAP Work?
CPAP stands for Continuous Positive Airway Pressure. The machine delivers a single, constant stream of air pressure that acts like a splint to keep your airway open while you sleep.
- Best For: Most patients with Obstructive Sleep Apnea (OSA). It is the “Gold Standard” first-line treatment.
How Does a BiPAP Work?
BiPAP stands for Bilevel Positive Airway Pressure. Unlike the CPAP, this machine alternates between two distinct pressure levels:
- IPAP (Inspiratory Pressure): Higher pressure when you breathe in to keep the airway open.
- EPAP (Expiratory Pressure): Lower pressure when you breathe out.
- Best For: Patients with high pressure requirements, COPD, or those who find it physically difficult to exhale against the constant force of a standard CPAP.
CPAP vs BiPAP: The Main Differences
While both look similar and use the same types of masks, their internal software functions differently:
| Feature | CPAP Machine | BiPAP Machine |
|---|---|---|
| Full Name | Continuous Positive Airway Pressure | Bilevel Positive Airway Pressure |
| Pressure Levels | Single, constant stream of air pressure. | Two distinct levels: IPAP (Inhale) and EPAP (Exhale). |
| How it Works | Acts like a splint to keep the airway open with a fixed flow. | Alternates pressure; provides higher pressure to inhale and lower to exhale. |
| Best For | “Gold Standard” for most patients with Obstructive Sleep Apnea (OSA). | High pressure needs, COPD, or those who find it difficult to exhale. |
Does Medicare Cover CPAP Machines?
Most people ask, “Does Medicare cover CPAP machines?” The answer is yes. Medicare Part B covers 80% of the cost of the machine and supplies (like masks and tubing) if you meet the clinical criteria.
- Note on BiPAP: Because BiPAP machines are more expensive, Medicare typically requires you to try a CPAP first. If the CPAP does not resolve your apnea, or if you cannot tolerate it, your doctor can then prescribe a BiPAP.
If you’re having trouble with your setup, our CPAP mask problems fixes guide offers practical tips to resolve leaks and discomfort.
The Path to Treatment: 4 Steps to Get a CPAP Machine
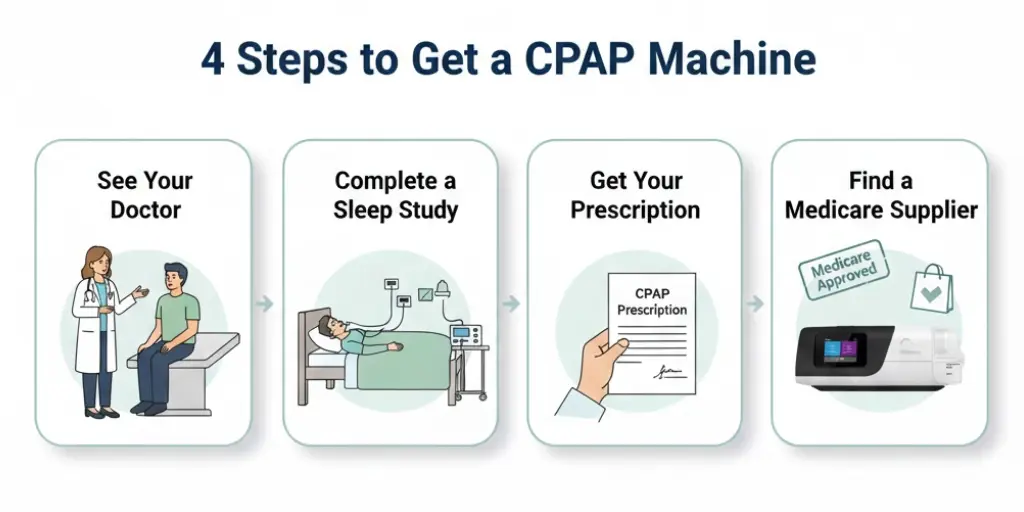
How to get a cpap machine through your insurance. Navigating insurance requirements can be confusing. Here is the standard process to get your CPAP or BiPAP covered by Medicare:
- See Your Doctor: You must have a face-to-face evaluation with your treating physician to document symptoms like snoring, fatigue, or gasping for air.
- Complete a Sleep Study: Your doctor will order a sleep test (either in a lab or a Home Sleep Test) to confirm your diagnosis of Obstructive Sleep Apnea (OSA).
- Get Your Prescription: Once diagnosed, your doctor will write a prescription for you.
Note: Medicare requires a specific “Standard Written Order” that includes the type of machine, pressure settings, and duration of use. - Find a Medicare Supplier: Reach out to authorized Medicare CPAP suppliers (like us!). We will collect your documents, verify your insurance eligibility, and set up your equipment.
Coverage Tip: Medicare initially approves a 12-week trial period. To keep the machine, you must use it for at least 4 hours a night on 70% of nights.
Find the Right Machine for Your Needs
Unsure which machine is right for you? Reach out today for a free consultation on how to get your sleep therapy equipment through insurance.
FAQ: CPAP vs. BiPAP & Medicare
Q1: What is the biggest difference between CPAP and BiPAP?
A: The primary difference is pressure delivery. A CPAP machine provides one continuous level of pressure. A BiPAP machine provides two levels: a higher pressure when you breathe in and a lower pressure when you breathe out, making exhalation feel more natural.
Q2: Does Medicare cover CPAP machines and their supplies?
A: Yes. Medicare Part B covers 80% of the cost for the machine and necessary supplies (like masks and tubing) once you meet the clinical criteria and your deductible.
Q3: Why does Medicare require me to try a CPAP before a BiPAP?
A: Because BiPAP machines are more expensive, Medicare guidelines generally require a trial of CPAP first. If the CPAP doesn’t work or you cannot tolerate the constant pressure, your doctor can then prescribe a BiPAP.
Q4: How many hours a night do I need to use my machine for Medicare to pay?
A: Medicare requires “compliance,” which means using the machine for at least 4 hours a night for at least 70% of the nights during your initial 12-week trial period.
Q5: What steps do I need to take to get a machine through insurance?
A: You must see your doctor for an evaluation, complete a sleep study (in-lab or at-home), receive a specific prescription called a “Standard Written Order,” and then provide these documents to an authorized Medicare supplier.